Sunday, November 30, 2008
Sunday, November 16, 2008
Posted by MS Gopalakrishnan at 11:33 AM 0 comments
Thursday, November 13, 2008
A reticent police officer
A reticent police officer has his way!
Posted by MS Gopalakrishnan at 1:40 AM 0 comments
Labels: Director's cut
Saturday, October 18, 2008
Invest in memory.
The other day we were trying to store operative videos in 1080p DVD quality from a Leica F40. A few hours and hundreds of gigabytes of video filled up all the hard disk space. If there is one area you would want to invest in, that would be memory storage solutions. Its only a matter of time before ordinary people video record their entire lives. Think about editing and retrieving information from all that data... a whole new breed of image and video search software would be needed.
Posted by MS Gopalakrishnan at 4:39 AM 0 comments
Labels: Just my thoughts
Thursday, September 18, 2008
There is strange peace when you give up your religion...
Its surprising but its true. Give up your religion and see what relief it brings! One would initially think that there will be turbulence and uncertainty... Religion is a strong initial programming... as strong and dear as your parents, assuming one was born in a highly religious family as most of us usually were.
Of course, giving up your religion is only a step away from escaping from the need to believe in God. Without regret, without fear, how many of us can question the concept of God that we were led to believe in?
Posted by MS Gopalakrishnan at 12:52 PM 1 Comment
Labels: Just my thoughts
Sunday, May 4, 2008
Tuberculum sella meningioma: subfrontal approach
25 year old lady was complaining of progressive diminution of vision since the last two years and had been investigated elsewhere with a plain CT scan one year back following referral by her ophthalmologist. She had completely lost her vision one year back during the last few months of pregnancy before the delivery of her first child. She has no other complaints.
On examination, she had no perception of light in either eye. Fundi had bilateral primary optic atrophy. There were no other deficits.
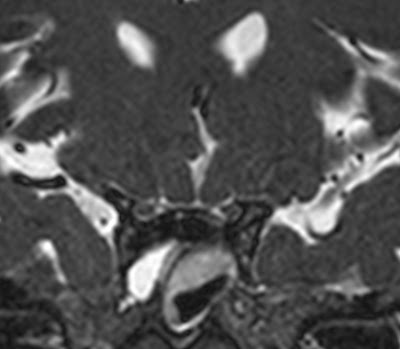
Plain CT scan [pvt film] showed a very ill defined small isodense suprasellar lesion. MRI showed a T1 isointense, T2 hyperintense lesion based on the tuberculum sellae stretching the optic nerve and chiasm. Lesion measured 3.0 X 2.6 X 2.3 cm. It was enchancing uniformly and brightly on Gad contrast. CT angiogram showed that the internal cerebral arteries and anterior cerebral arteries were stretched out but not encased by the lesion.
Since there was little possibility of recovery of vision even after microsurgical removal of the tumor in view of long standing total visual loss and established optic atrophy, she was strongly encouraged to consider the option of getting Gammaknife radiosurgery at concessional rate at another hospital. However, she and her husband chose to have microsurgery. She had developed phenytoin rash prior to surgery and anticonvulsant treatment was switched over to sodium valproate.
On 8/04/08 she underwent bifrontal craniotomy, sub frontal approach and complete excision of the lesion. [M.S. Gopalakrishnan, V.S. Hari, Balasubramanium] A sinusoidal bicoronal stealth incision was used for good cosmesis. An initial pterional transylvian approach had to be changed to bilateral subfrontal approach in view of technical (maneuvering) difficulties encountered with the available operating microscope. The lesion was firm and moderately vascular. A very small part of the lesion which was densely adherent to the left

Patient developed drowsiness on post operative day eight which improved with intensification of antiedema measures. Post op CT scan showed complete excision of the lesion. Bilateral basifrontal edema was present [retraction induced]. Pseudo-meningocele was aspirated and pressure dressing was given. At the time of discharge, she is afebrile, and well oriented. However she has increased talkativeness which may be due to mild frontal disinhibition due to frontal lobe retraction. This is expected to resolve.
Histopathology report is menigothelial meningioma [WHO grade 1]
Discussion:
The plain scan:

Posted by MS Gopalakrishnan at 10:17 AM 0 comments
Labels: operative cases
Lacrimal gland adenoid cystic carcinoma recurrence

64 year old gentleman was diagnosed to have lacrimal gland adenoid cystic carcinoma following excision of a mass under the right eyebrow, via lateral orbitotomy, done in a hospital elsewhere in March 2004. Following that he presented in ophthalmology OPD with a firm lobulated mass in right eye below eyebrow. A biopsy was done, which confirmed the diagnosis. He completed radiotherapy in 23/12/08 since further surgery was deemed not possible at that time.
[40 cGy in 20 fractions, field size 15X6 cms to right eye, tumor depth 4 cms, 24 cGy in 12 fractions, right anterior and right lateral fields with wedges and left eye shielded].
In 24/1/07, the tumor recurred. [FNAC 572/07] and in 24/06/07 he underwent local re-excision of the mass.
In 28/1/08 he presented with pain and bleeding from right eye and was evaluated with a CT scan which showed tumor recurrence. He had undergone cataract excision and intraocular lens placement in left eye in 12/2/08. On examination he had a firm mass felt under the lateral aspect of right eyebrow, with surrounding edema causing ptosis and chemosis in right eye. There was no useful vision in right eye.
Ct scan had revealed an enhancing lesion in the right orbit lateral to the globe which was eroding the roof and lateral wall of the orbit. Metastatic work up was negative.
On 23/2/08 he underwent exenteration of the right orbit[ophthal], followed by excision of the roof and lateral walls of the orbit after a right fronto-temporal craniotomy [neurosurgery. The firm tumor, the involved orbital ridge and a margin of bone up to the orbital apex were excised. A few areas of inadvertent dural tears were repaired using pericranial patch. Frontal sinus was exteriorized. Temporalis muscle was placed in the socket and a local rotation flap was used to cover the bare socket. [plastic] Post operatively he had a few episodes of CSF rhinorrhea which settled with lumbar drainage.
Post op CT scan had showed complete excision of the tumor and bone excision up to the orbital apex.
After one and half months of discharge from hospital he presented with purulent discharge from right nostril with tenderness in right maxillary sinus area. This was treated with sinus washes and antibiotics. He complained of occasional episodes of clear watery discharge from right nostril suggestive of CSF rhinorrhea. This tended to occur in right lateral position as he gets up from sleep.
He was re-admitted for evaluation and treatment of possible CSF rhinorrhea. An MRI with Ciss 3d sequence could not reliably pick up a site of leak. So he underwent lumbar puncture and intra-thecal contrast cisterography in prone position to identify site of leak. This investigation also failed to reveal a leak. He was on lumbar csf drainage for five days prior to contrast cisternography . The CSF sample which was taken on the last day prior to removing the catheter had plenty of pus cells and grew acinetobacter sensitive to meropenam, amikacin , ceftazidime and ciprofloxacin. He also had headache and mild meningeal signs. Meningeal signs and fever settled with meropneam [given initially for three days] and other sensitive antibiotics. Csf leak also disappeared.
At discharge he is afebrile, ambulant and comfortable.
Discussion:
Patient had recurrence of lesion after initial surgery, radiation therapy and re-excision. An oncologically adequate resection required excision of the tumor and in addition, the involved orbital bone with adequate margins. This necessitated a fronto-temporal craniotomy followed by excision of the roof and lateral walls of the orbit up to the orbital apex after exenteration of the eye. This should maximize the chances of complete tumor excision and minimize risk of further recurrence of this type of highly malignant tumor.
Symptoms suggestive of delayed leak were reported by the patient. However the site of the leak could not be ascertained by either a ciss 3d sequence of mri or by contrast cisternogram. Hence a direct repair could not be carried out. Also the leak never occurred during hospital stay after initiation of csf drainage. It is possible that the leak is not detected since it is intermittent. Patient developed meningeal signs after removal of the csf catheter [iatrogenic or as a result of unapparent csf rhiorrhea]. This resolved within a day of starting antibiotics. Also the leak seems to have spontaneously resolved. If leak recurs in future, a lumboperitoneal shunt procedure may be carried out as site of leak is obscure to do an anatomical repair. Intradural exploration, re-exterioirization of frontal sinus, anterior fossa carpeting with a large pericranial or fascia lata graft can also be considered as an alternative.
He requires careful and regular imaging follow up to rule out tumor recurrence.
Posted by MS Gopalakrishnan at 9:25 AM 0 comments
Labels: operative cases
Sunday, April 27, 2008
Giant acoustic schwannoma

Things cant be worse. After operating for almost 24 hours, [stage one: 10: 45 am to 10 pm, stage two: 10: 15 am to 11 pm] it still isn't complete! The broad relation to the brainstem needs to be dissected and i am not even sure how much tumor is left.
Tumor was firm, fibrous and vascular [pluckable]. Dissection of the facial nerve took around three hours.
Just thinking of my 'dissection velocity' ... a tuberculum sellae meningioma of 3.0 cm maximum diameter took around 12 hours. The consistency and vascularity and general difficulty were comparable. The vestibular schwannoma with a maximum diameter of 5.2 cm, has a surface area that is almost three times that of the smaller tuberculum sellae meningioma. Its volume should be around seven times larger. [ surface area is a function of square of the diameter, volume is a cube of the diameter] .
tumor decompression must be a function of the surface area [the stretched out normal structures which one has to protect] and volume [the tumor one has to internally decompress], if everything else remain constant [like surgeon experience, location, consistency, vascularity etc]
i shudder to think how many more hours will be required. Wish i had a dedicated neuromicroscope. Every adjustment of the present microscope [borrowed from plastic surgery] takes 20- 30 seconds and can even extend up to a minute. The eyepiece is not tiltable and visualisation is poor. A good microscope should cut down the time by half. so will a CUSA and nerve stimulator.
I will put up the post op scan. This is indeed a long nightmare.
Posted by MS Gopalakrishnan at 5:43 AM 0 comments
Labels: Suboptimal results
Monday, January 28, 2008
Trans-lamina terminalis approach for sellar suprasellar craniopharyngioma
Twelve year old girl with bitemporal hemianopic defect. Hormonal values are normal.
Thinking of translamina terminalis approach versus pterional or both! May be drill the tuberculum sella also.
Hope everything goes fine... [I would have waited for a better microscope, but her parents are getting increasingly desperate after visiting four different hospitals. Any more delay, they might not come back]
Outcome:
Ok, As planned: Sinusoidal stealth incision for Souttar like flap , bifronto-right temporal craniotomy [keeping open the option of right pterional approach], dissection of optic tracts, basal interhemispheric dissection, translamina terminalis approach, switch to right pterional approach. Abdominal fat graft was taken thru umbilical incision.
Problems:
Small dural tear at the burr hole site. The new Midas rex gold legend [first time I am using this] has to be used carefully if you are using the acorn head for making a burrhole. No perforator attachment was bought.
Lost an olfactory tract during early part of tumor decompression. [Preserving the tract is an indicator of the gentleness of retraction, dissection and surgery in general]
Quite satisfactory excision could be achieved after opening the LT. Basilar bifurcation and stalk could be seen after tumor removal.
However, the retrochiasmatic and sellar part of the tumor could not be well visualised. [this was expected.] See diagram: the red line is the line of sight if one doesnt take the eclipsing tuberculum sellae out. The blue is perhaps what it would be after removing the yellow outline of tuberculum sellae

Tried to take the retrochiasmatic part after taking the pterional route basically using the carotico- optic space, but wasnt so effective. Thought abt drilling of the tuberculum to access the sellar part through below the chiasm. [Why didnt I? May be "end-of-surgery-apprehension syndrome": Will I injure the chiasm using the drill?]
Post op: Recovered well remarkeably. Thought she might have severe hypothalamic disturbance. Required a few doses of vasopressin for two days. Then urine output decreased. [? triphasic response]
Postop scan after around eight days:


Exactly as expected: Enhancing tumor residue in the sella and just above. Notice the flow void through the floor of the third ventricle.
Plan now: IMRT/conformal RT
Or may be re-excise extended trans-sphenoidal??
Conclusion: Lamina termianlis approach isnt the shortest way to reach the tumor [cf pterional, transylvian] but it is quite versatile and straight forward. Ill persist to use multiple approaches [all possible approaches if needed] simultanously. Wouldnt hesitate to drill that eclipsing tuberculum.
Great article to read:

Posted by MS Gopalakrishnan at 8:20 AM 0 comments
Sunday, January 13, 2008
Spontaneous CSF rhinorrhea - MRI CISS images - cribriform plate defect



The defect in the cribriform plate was quite small. The olfactory bulb and tract were lying free without attachment to the plate on the affected right side. The olfactory bulb and tract were preserved on the left side. [could have almost got sucked away at one point].
Bicoronal sinusoidal stealth incision - bifrontal craniotomy. [cosmetic reasons]
Abdominal fat graft and vascularised pericranial graft onlay on both sides. [just to be totally sure...]
Post op: no leak. olfactory function preserved.
Posted by MS Gopalakrishnan at 7:22 AM 0 comments








